As an organization that once hosted many in-person programs to aid and empower diverse communities, my host site has adjusted to new circumstances to continue to advocate and serve Philadelphia.
showed me how to apply motivational interviewing skills,
facilitate effective conversation, and
motivate participants on their health journeys.
Across Philadelphia’s diverse neighborhoods, hypertension and diabetes are two chronic diseases that have high incidence rates amongst community members. While treating a disease can be a seemingly scientific approach, my time with the Frazier Family Coalition at Jefferson has demonstrated that there are so many complex factors involved in how a patient may develop and experience disease. Working with underserved populations in North Philadelphia has demonstrated that understanding context and evaluating social determinants of health (SDOH) are just as important as assessing the symptoms of the disease.
Serving at my host site has provided me the opportunity to help analyze the socioeconomic needs of the communities that the Coalition serves, while also providing insight into the challenges that Philadelphians may face to attend to their health. While I was aware that access to transportation and affordable healthy food were major barriers to a patient’s health, I did not realize that other issues, such as the ability to read hospital materials, the ability to speak English, the safety of one’s household, and access to childcare can compound with other immediate needs. These overlapping and compounding issues can make it difficult for a patient to put their health and wellbeing first. Alongside the nurse navigator and the community health workers at my host site, I also help assess patient’s various non-medical needs and refer them to resources to lighten the load in hopes that the patient can address their health needs.

have served so many people, and serving virtually
has allowed us to serve even more!
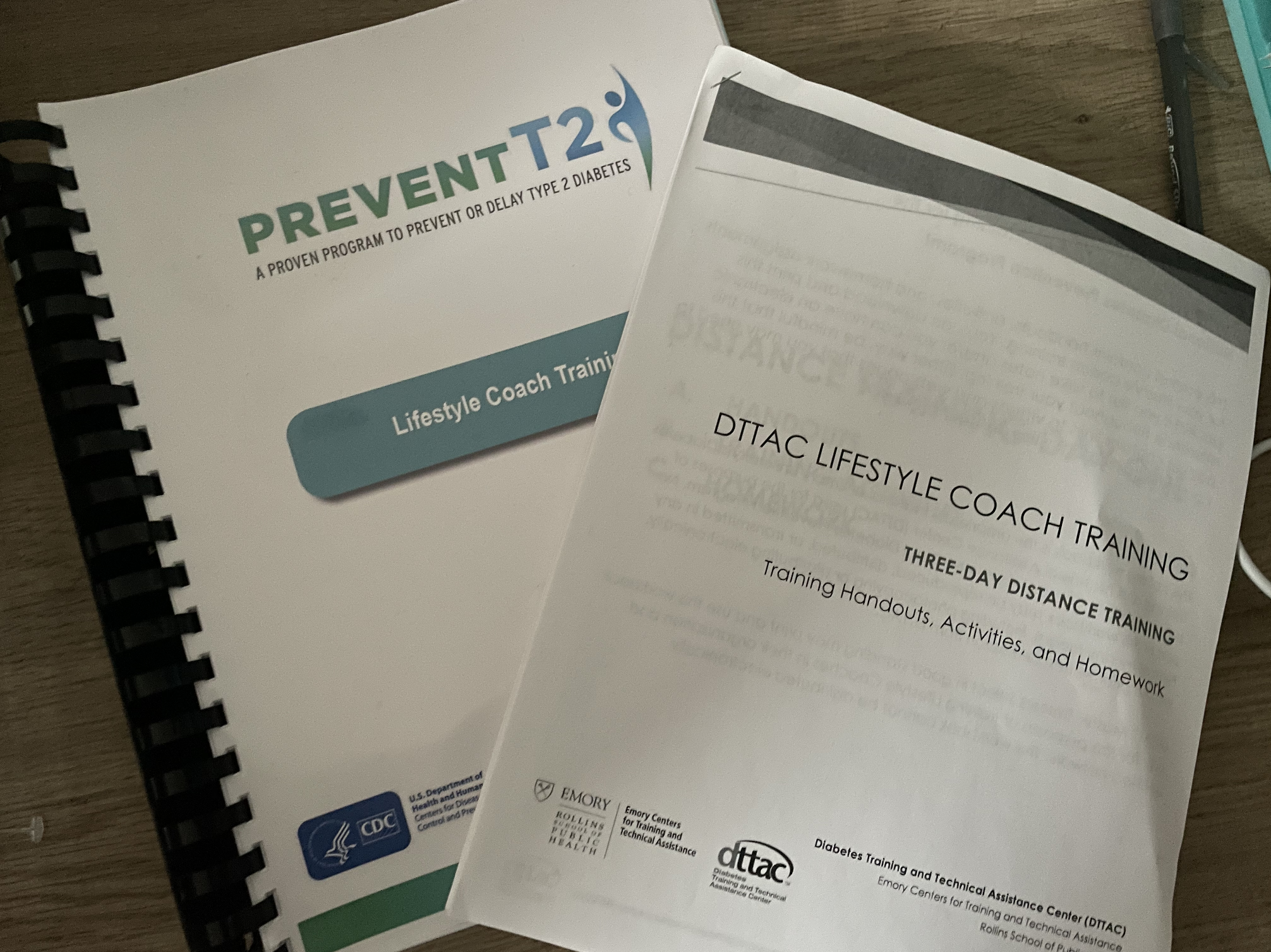
At the Frazier Family Coalition, we offer several classes and webinars to address the high incidence rates of these chronic diseases. With my host site, I have been able to teach my own Diabetes Prevention Program class. Through this program, we aim to help those at highest risk of diabetes reduce their risk of the chronic disease through empowerment and implementation of lifestyle changes. One thing that I appreciate about the program curriculum is that it isn’t extreme and encourages participants to make moderate changes. For example, rather than telling program participants to run a mile once a week, they can walk around the mall or the grocery store for 30 minutes, or stand instead of sitting during commercial breaks when watching tv. Being a lifestyle coach has also helped me really connect with members of the class; as I see them every week, learn about how their week was spent, what they did last weekend, and new recipes they learned, I find myself completely invested in their success in the program. It is also exciting to see members of the class connect with each other, share their experiences, and compare tips to succeed on their health journey. I feel like I’ve made an impact.
While I am past the halfway point in my service term, I’ve learned so much about healthcare, public health, and working collaboratively with community members and leaders. I am extremely grateful that National Health Corps has given me the chance to work with Jefferson in this context. Working with vulnerable communities, especially through connecting with them as a lifestyle coach every week, has been extremely fulfilling and has immersed me in the value of patient advocacy. Through patient interactions especially in evaluating social determinants of health, I’ve understood that context is extremely valuable in order to provide comprehensive care. As a future physician, I will be sure to apply these skills as I care for the diverse patient populations that I hope to serve.
