 |
|
Implant |
I was recently caught off guard by a student’s comment at a teen pregnancy prevention class at Lone Star High School. I always facilitate my teen pregnancy prevention classes by discussing the methods of birth control in order of effectiveness, since teenage attention spans are infamously short. I start by discussing abstinence, since not having sex is the only 100% ensured way not to get pregnant. Then, I move on to the Long Term Reversible Contraceptive Methods (LARCs), which are the most effective methods of birth control available on the market today. Though this class is super important in these teens’ lives, the material can be a lot to take in and overwhelming. I do my best, but the reality that any teacher faces is that teens often check out during health class. That wasn’t true on this particular day, however.
Though LARC methods have been around for many years, there is a lot of misinformation out there, so let’s go through the basics. There are two main kinds of LARCs—the Implant and the Intrauterine Device (IUD). The Implant is a small match-stick sized piece of plastic which releases the hormone progestin into the upper arm and protects a person from pregnancy for three years. All IUDs are small, T-shaped pieces of plastic that work to prevent pregnancy by releasing the hormone progestin (hormonal IUD) or changing the chemistry of the uterus using copper wire (non-hormonal IUD). The Skyla and the Mirena are the two hormonal IUDs which provide pregnancy protection for three and five years, respectively. The Skyla method is smaller in size than the Mirena, contains a slightly lower dose of progestin, and is FDA approved for use in people who have not yet had children. The Paraguard, or the non-hormonal IUD, provides pregnancy protection for up to 12 years. A person can get their IUD removed by a healthcare provider at any time and restore their ability to get pregnant. These methods provide very effective long-term protection against pregnancy and take the risk for human error in use out of the equation.
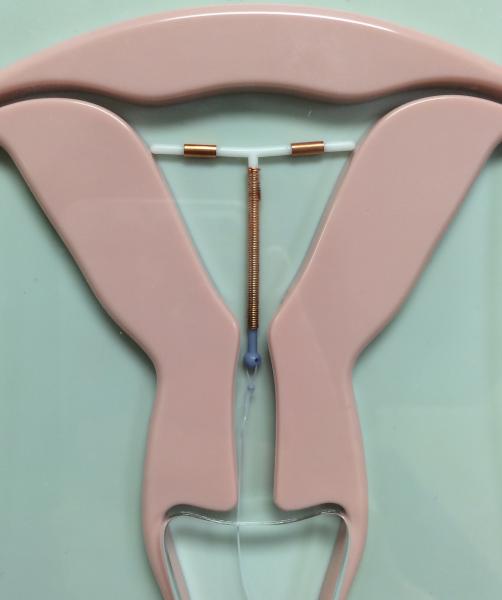 |
| IUD |
Though I try to be unbiased in my comprehensive family planning education, I truly do feel strongly that teens should know what LARCs are, how they work, and why they’re beneficial. I believe these methods are easier for teens to handle—there’s no pill to remember to take at the same time each day, no patch to change each week, no ring to change monthly, and no shot to get quarterly. In fact, a study recently confirmed that teens have higher compliance rates with LARCS than they do with other methods after a year of use.1 Evidence that LARCs make a real difference in reducing the number of teenage pregnancies can be found in the recently published results of the Contraceptive CHOICE Project in the New England Journal of Medicine. This study found that after two or three years of use, teens that used LARC methods had lower rates of unintended pregnancy, teen birth, and abortion than the average rates for American teens.2 Since the publication of that study, groups like the American College of Obstetricians and Gynecologists and the Physicians for Reproductive Health have officially released statements advocated for teenage usage of LARCs.3,4 Clearly, a lot of people are on-board with the idea that LARCs are a great method for teens to use to prevent unintended pregnancy, but the reality is that only an estimated 1.6% of American teens use LARCs as their birth control method.5
So, what did that student say in the middle of my lesson? She asked me, “Why don’t all girls get a LARC?” I was taken aback. After one, introductory class about this birth control method, this student asked the core question that is puzzling both sexual health educators and doctors alike. The choice to use an IUD seems almost common sense, considering the ease of use and high efficacy rates, but why the reluctance? Why the push back? I recently came across a surprisingly poignant article in Cosmopolitan Magazine that was trying to probe at this exact question. The article cited reasons such as lack of understanding by both patients and physicians, ugly memories of a since recalled IUD (the Dalkon-Shield) that resulted in 17 deaths in the 1970s, marketing of the IUD to only married people who had already had babies, and TV commercials from law firms looking for people who face the rare side effect of perforation of the uterus by the IUD for the low rates of LARC usage. It also detailed first-hand accounts from both female teens and doctors about their thoughts on the method choice, insertion process, and recovery, allowing providers the chance to clear up misconceptions and anxieties about LARCs.6 I was amazed by how upfront this mainstream publication was about the issue of LARC use in teens; in truth, it goes to show how important this conversation is on a national stage. If we as a society want to reduce the number of unintended teen pregnancies, we need to dispel these myths about LARCs and really start promoting LARC use in teenagers.
Citations
1. Peipert, J., T. Madden, J. Allsworth, Q. Zhao, D. Eisenberg, and G. Secura. "Continuation and Satisfaction of Reversible Contraception: A Preliminary Analysis from the Contraceptive CHOICE Project." Contraception 5 (2011): 193-94. Print.
2. Secura, Gina, Tessa Madden, Colleen McNicholas, Jennifer Mullersman, Christina Bucknel, Qiuhong Zhao, and Jeffrey Peipert. "Provision of No-Cost, Long-Acting Contraception and Teenage Pregnancy." The New England Journal of Medicine 371 (2014): 1316-323. Print.
3. Adolescents and long-acting reversible contraception: implants and intrauterine devices. Committee Opinion No. 539. American College of Obstetricians and Gynecologists. Obstet Gynecol 2012;120:983–8.
4. Morrell, Kathleen. "Physicians for Reproductive Health." Prh.org. Physicians for Reproductive Health, 18 Nov. 2014. Web. 21 Feb. 2015. <">http://prh.org/larc-awareness-week-teens-smart-birth-control-option/>.
5. Frieden, T., H. Jaffee, J. Cono, et al. [Youth Risk Behavior Surveillance—United States, 2013.] MMWR 2014; 63(No. SS-4):[27].
6. Maltby, Anna. "Should You Get an IUD?" Cosmopolitan. Hearst Digital Media, 15 Feb. 2015. Web. 21 Feb. 2015. <">http://snip.ly/XWLW#http://www.cosmopolitan.com/health-fitness/a35806/sh....

This blog post was written by NFHC member Molly Spilka.
Molly serves at FDOH-Duval as a Preconception/Interconception Health Educator.
