Closing the Digital Divide, One Patient At A Time
As a public health major in college, I heard the terms'social determinants of health" and'health disparities" a lot. For anyone unfamiliar with this sort of jargon, these terms are often used when referring to the different sociocultural, political, and historical factors that contribute to the existence of unequal health outcomes on a societal level. The field of public health has seen a near-simultaneous theoretical restructuring in recent years, with increasing emphasis on the role of factors such as race, socioeconomic status, sexual orientation, and geographic location over the more traditional focus on individual actions. In 2011, the CDC affirmed this conceptual shift with the inaugural publication of the Health Disparities & Inequalities Report, with its express aim to'identify and address the factors that lead to health disparities… so that barriers to health equity can be removed."
This push towards studying structural factors makes intuitive sense. After all, public health cannot simply be reduced to the consequences of individual behavior - adequately understanding and responding to current health issues requires also examining the systems and institutions in which individuals exist. The primary limitation, however, with this collective shift in mentality has to do with the fact that structural factors are far more difficult to define and analyze. How does one begin to label every complex, intersecting form of identity found in the world? The simple answer is: you can't. As such, the public health field has zeroed in on a few key social determinants (think race, gender, socioeconomic status) - and sometimes at the expense of others.
One such example that has taken on particular relevance to me this service term is the phenomenon of the digital divide. What this refers to is the differential access to and use of the many forms of technology prevalent in the United States today. If you're reading this blog, you likely belong to one side of the digital divide - the one which automatically routes all inquiries to Google, and illegally downloads their music. But the fact of the matter is, for those of us fortunate enough to be able to even understand the term'Netflix and chill", there is an entire subset of the American population that does not own a smartphone. As the Baltimore-based writer and scholar D. Watkins wrote on the digital divide,'I love that our country is a leader in innovation, but why can't we be leaders in assuring that all of our citizens can enjoy our accomplishments?"
While it may not be immediately apparent how this discrepancy relates to health, think about how the Medicaid/Medicare expansions created by the Affordable Care Act are most easily accessed through the Healthcare.gov website. Or think about how governments around the world are increasingly turning to text updates to keep citizens safe during the event of a natural disaster.
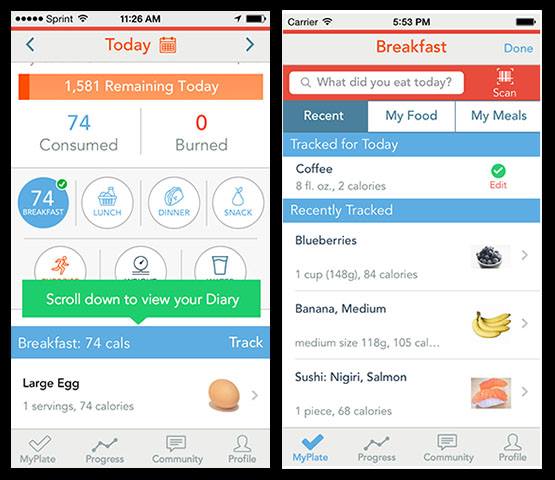
In my service as a Health Navigator, I work to close the digital divide, albeit on a much smaller scale. I have been actively involved with creating and presenting educational materials for the new weight loss clinic, where I will soon begin teaching a class on using the MyPlate weight loss app to supplement and support the efforts of the nutritionists and primary care physicians. While many of the patients that I work with have expressed low levels of familiarity or comfort with using a smartphone, all are willing and excited to learn. Using a weight loss app not only helps with the practical requirements of meal and exercise tracking - it also provides users with a greater sense of personal control over their health. Because that's the other piece related to technology - it has the capacity to empower users, not merely serve them. And when it comes to public health, empowerment has to be the end game in order for health equity to be possible.

This post was written by NHC Chicago Member Anne Lin. Anne serves as a Health Navigator with Smart Chicago Collaborative at Fantus Health Center.
